57
- hacking-medschool/septic-arthritis
- Septic arthritis Medscape
- youtu.be/oecTN_y37Y4
- youtu.be/D6fbEadTt9o
Osteomyelitis
Osteoporosis
(osteoporosis and metabolic bone disease are included here andunder Rheumatology)
NHS Consensus Development Conference Definition
a progressive skeletal disorder characterised by low bone mass and microarchitectural deterioration of bone tissue with a consequent increase in bone fragility and susceptibility to fracture
WHO Definition
osteoporosis: bone density greater than 2.5 SD below the mean (femoral neck)
osteopenia: bone density greater than 1 SD below the mean
One definition is a pathological process and the other is an arbitrary point on a scale (source GP Update?)
T-score criteria were proposed for epidemiological studies to compare populations and for defining thresholds in clinical trials.
They were not intended for diagnosis or management decisions in individual cases.
Risk factors
- postmenopausal women
- early menopause (before 45 years of age, e.g. following a hysterectomy or oophorectomy)
- immobility
- long-term steroid use (it is suggested that this group receive preventative treatment)
- previous fragility fracture
- high systolic BP (higher rate of bone loss)
- secondary causes will affect up to 50% of men and 10% of women with osteoporosis
- eg alcoholism
- thyroid problem ( both hypothyroidism and hyperthyroidism)
- liver disease
- GI malabsorption
- hypogonadism in men
- connective tissue disorders (e.g. rheumatoid and SLE
Osteoporosis guidelines
Osteoporosis FRAX
Osteoporosis Screening
- NICE TA160 1ry prevention
- NICE TA161 Jan 2ry Prevention
- National Osteoporosis Society
- FRAX
- SIGN 71 Osteoporosis
Royal College of Physicians guidelines for DEXA scanning 1999/2002
History of fragility fractures
Kyphosis and loss of height due to vertebral crush fracture confirmed by radiography (people with a history of two or more vertebral fractures are automatically considered to be at high risk and should be started on prophylaxis without waiting for a DEXA scan)
Radiographic evidence of osteopenia or vertebral deformity
Oral steroids at any dose for >3 months (unless >65 or previous fragility fracture then start prophylaxis regardless)
Premature menopause <45
History of amenorrhoea for> 1 year
Primary hypogonadism
Chronic disease associated with osteoporosis, eg rheumatoid arthritis, hyperthyroidism, Crohn’s disease, coeliac disease, alcoholism, anorexia nervosa
Maternal family history of hip fracture
Body mass index (BMI) <19 kglm2.
Osteoporosis secondary prevention
| Causes of secondary osteoporosis |
|---|
| type I (insulin dependent) diabetes |
| osteogenesis imperfecta in adults |
| untreated long-standing hyperthyroidism |
| hypogonadism |
| premature menopause |
| chronic malnutrition |
| malabsorption |
| chronic liver disease |
all women over 75 years who have fractured should be treated for presumed osteoporosis without the need for a DEXA scan
all women between 65 and 74 years of age should be treated if osteoporosis is confirmed by DEXA scan
women younger than 65 years should be treated:
if they have a bone mineral density less than -3 SD
if they have a bone mineral density of -2.5 SD with one or more additional risk factors (BMI less than 19kg/m2, a family history of maternal hip
fracture if less than 75 years of age, untreated premature menopause, medical disorders associated with bone loss or conditions associated with prolonged immobility).
For treatment, NICE’s preference is the bisphosphonates with raloxifene as an alternative.
Teriparatide should be restricted for use in more severe cases.
Osteoporosis treatments
Prevention/lifestyle changes
Stop smoking, avoid excess alcohol and take regular weight-bearing exercise.
Fall prevention assessment of safety in the home can be provided in primary care.
Protection of sites of high impact hip protectors are of proven benefit, with up to 50% reduction in some studies (residential care based).
See NOGG Pocket Guide for Healthcare Professionals and NICE TA161
Bisphosphonates
These are now first choice in management of osteoporosis. A once-monthly preparation, ibandronate, has recently been released. Bisphosphonates have been
identified as a cause of osteonecrosis of the jaw (one to three years after starting treatment)
There is most evidence for alendronate (in men and women) and risedronate (in women only). Patients who have had a history of achalasia or strictures, or
those who cannot tolerate these drugs could be offered cyclical etidronate. However, unlike alendronate and risedronate, etidronate does not reduce the
risk of non-vertebral fractures. Age alone should not be a reason to withhold bisphosphonates, but they are not routinely prescribed for women of childbearing
age or for pregnant women. Patients should be advised that bisphosphonates are very poorly absorbed and must be taken on an empty stomach in order to maximise their absorption.
FIRST CHOICE: ALENDRONATE 70mg weekly
Alendronate (alendronic acid) tablets 10mg, 70mg
Dose: Treatment of postmenopausal osteoporosis and osteoporosis in men, 10mg daily or (in postmenopausal osteoporosis) 70mg once weekly. Prevention of postmenopausal osteoporosis, 5mg daily. Prevention and treatment of corticosteroid-induced osteoporosis, 5mg daily (postmenopausal women not receiving HRT, 10 mg daily).
Risedronate (risedronate sodium) tablets 5mg, 35mg
Dose: Treatment of postmenopausal osteoporosis, 5mg daily or 35mg once weekly. Prevention of osteoporosis (including corticosteroid-induced osteoporosis) in postmenopausal women 5mg daily.
In the case of both alendronate and risedronate, patients should be counselled to swallow tablets whole with a full glass of water on an empty stomach at least 30-60 minutes before breakfast, and to stand or sit upright for at least 30 minutes afterwards. Risedronate may be taken at other times of the day as long as it is at least 2 hours after last food and drink. However, tablets should not be taken at bedtime or before rising. Calcium and vitamin D supplements should be co-prescribed with bisphosphonates. Products containing calcium, magnesium, aluminium or iron should be taken at a different time of day to risedronate.
Oral bisphosphonates should be used with caution in patients with active or recent oesophageal or upper GI problems. Alendronate is contraindicated, and risedronate should be used with caution, in patients with abnormalities of the oesophagus or factors delaying oesophageal emptying. Alendronate is not recommended in patients with eGFR<35mL/min due to lack of data. Risedronate is contraindicated by the manufacturer in patients with eGFR<30mL/min, however the Renal Drug Handbook advises that risedronate may be dosed as in normal renal function in patients with eGFR 20-50mL/min. Use of bisphosphonates in patients with eGFR lower than recommended should be discussed with a Renal specialist.
Zoledronic acid annual intravenous infusion, 5mg (Aclasta®) is a hospital-only bisphosphonate for the treatment of osteoporosis in post-menopausal women at increased risk of fractures.
Osteonecrosis of the jaw has been reported in association with bisphosphonates. Most reports have been in patients treated with intravenous bisphosphonates; however, reports have also been received in those taking oral bisphosphonates. Patients should be advised to inform their dentist that they are receiving bisphosphonate therapy prior to dental treatment. A dental examination with appropriate preventative dentistry should be considered prior to treatment with bisphosphonates in patients with concomitant risk factors (e.g. cancer, chemotherapy, radiotherapy, corticosteroids, poor oral hygiene, and gum disease). Adequate oral hygiene should be maintained during and after treatment with bisphosphonates.
Atypical stress fractures of the proximal femoral shaft have been reported in patients treated long-term with alendronate. Patients who develop stress fractures should discontinue alendronate and receive no further bisphosphonate treatment unless the benefits for the individual clearly outweigh the risk of harm. An increased risk of atypical fractures with other bisphosphonates cannot be excluded.
Other drugs affecting bone metabolism
Strontium ranelate
This is a dual agent (like teriparatide) that improves bone mineral density by increasing bone formation and reducing bone resorption.
Strontium ranelate works by suppressing the action of osteoclasts and by stimulating osteoblasts. Its precise place in treatment is not well established
and there have not yet been any studies comparing it with other osteoporosis medications in terms of effectiveness in reducing the risk of fractures.
sachets, 2g may be considered as an alternative to bisphosphonates for the treatment of postmenopausal osteoporosis in women at high risk of fracture, equivalent to age over 75 years with a previous fragility fracture and a T-score of < -2.4, in whom bisphosphonates are contraindicated or not tolerated.
Raloxifene
Raloxifene is an alternative to the bisphosphonates, but does not reduce the risk of non-vertebral fractures; it does, however, protect against breast cancer,
although there is an increased risk of thromboembolic disease associated with its use. In their draft guidance, NICE recommends it for secondary
prevention in women for whom bisphosphonates are contraindicated, for those who are physically unable to take a bisphosphonate in the
recommended manner, and for women who have had an inadequate clinical response to, or who are intolerant of, bisphosphonates. A clinically
inadequate response is defined as sustaining a further fracture even after 2-3 years of adequate treatment.
hydrochloride tablets, 60mg may be useful where bisphosphonates or strontium ranelate cannot be used.
Denosumab (Prolia®?) is a human monoclonal antibody that inhibits osteoclast formation, function, and survival thereby decreasing bone resorption. It is restricted to use in patients with a bone mineral density (BMD) T-score < -2.5 and ? -4.0 for whom oral bisphosphonates are unsuitable due to contraindication, intolerance or inability to comply with the special administration instructions.
Calcitonin
Calcitonin (used intranasally) is a newer medication. However, it is very expensive and has not been shown to reduce the risk of non-vertebral fractures.
Parathyroid hormone (teriparatide Forsteo®)
Parathyroid hormone (teriparatide) was approved in the UK for the treatment of severe osteoporosis in postmenopausal women in June 2003. The recommended dose is 20 IJg administered once daily by subcutaneous injection into the thigh or abdomen. Patients taking teriparatide must receive training on the injection technique. The maximum total duration of treatment should not exceed 18 months, because of concerns about its carcinogenic potential (in rats only!). NICE recommends that it should only be used in
secondary prevention of osteoporotic fractures for women >65 who have not responded to treatment with bisphosphonates (or who are intolerant to them)
and who have a very high fracture risk (T score <-4.0; or <-3.0 if there is a history of multiple fractures plus one or more of the following risk factors:
maternal history of hip fracture under the age of 75, 8MI <19 kglm2, prolonged immobility or untreated premature menopause).
(recombinant fragment of parathyroid hormone) and recombinant human parathyroid hormone (Preotact®?) are both subcutaneous injections that are indicated for severe osteoporosis within a specialist treatment pathway.
Calcium and Vitamin D supplements
Calcium (600-1200 mg daily) and vitamin D (400-800 units daily)
supplements are often given in conjunction with bisphosphonates, particularly if the patient has a poor diet. All frail and housebound patients (eg in nursing
and residential homes) should probably be considered for treatment. NICE advises that, ‘unless the clinician is confident that women who receive
osteoporosis treatment have an adequate calcium intake and are vitamin D replete, calcium and/or vitamin D supplementation should be provided.
Calcium
1 gram for people over 50 years of age.
There is no evidence that calcium reduces fractures unless it is taken with vitamin D.
Vitamin D
The recommended daily dose is 400 iU, too low for fracture prevention.
More usually, 800 iU would be used.
Two trials have shown that vitamin D and calcium reduced risk of fracture by up to 50% over five years. The best results are seen in institutionalised frail elderly.
Hormone replacement therapy
A meta-analysis suggests that this yields a relative risk reduction of 40% (for fractures). However, the benefits are lost within five years of stopping HRT. This
is a treatment option that is no longer recommended for prevention because of the risk factor profile.
Tibolone (bleed-free preparation of HRT)
This has been shown to increase bone mass density in the spine over two years.
Selective oestrogen receptor modulators (e.g. Raloxifene)
These decrease the fracture rate by 30% over three years at best.
Hormone replacement therapy (HRT)
HRT may be considered if a woman is symptomatic from the menopause and has osteopenia, but it is not licensed to treat established osteoporosis.
Steroid induced osteoporosis
- Steroid-induced Osteoporosis PUK
- Steroid induced osteoporosis CKS
- Oxford journals Steroid Osteoporosis
- washington.edu Steroid Osteoporosis
Osteomalacia
- youtu.be/0ske4pkcvxQ
- youtu.be/LlvMOB-Idgw
- youtu.be/HNm8Mzzb-U0
- Osteomalacia PUK
- Osteomalacia and Rickets PUK
Rickets
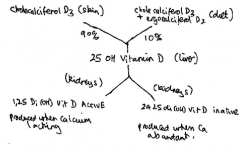
Vitamin D metabolism
Pagets bone disease
Causes deformity of legs (bowing) skull (enlarged calvarium with corrugated scalp) and other bones eg pelvis humerus clavicles – causing bone pain, pathological fractures, cranial nerve pasies (esp CN8) osteogenic sarcoma and high output CCF.
Biochemical markers in bone disease
biochemical markers