36
- British Thoracic Society Guidelines
- RCGP respiratory e-learning
- Dundee Chest
- Rural Health West Aug 2011 Respiratory
- http://youtu.be/YPz8bVR_Uio
- http://youtu.be/mMQsZimjayI
- http://youtu.be/bklrcFuiH-8
- Pulmonary 1 Seattle Pacific University iTU
- Pulmonary 2 Seattle Pacific University iTU
- Pulmonary part 3 Seattle Pacific University iTU
| Respiratory anatomy and physiology |
|---|
| Respiratory Physiology Dr F Roberts nda.ox.ac.uk |
| Respiratory history and exam |
|---|
Patterns of breathing
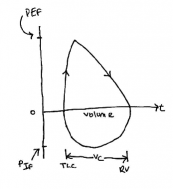
| Lung volumes and spirometry | |
|---|---|
| Tidal Volume | Volume of air moved during quiet respiration |
| Forced Vital Capacity FVC | Volume expelled by a forced exhalation from a maximal inspiration |
| Functional Residual Capacity FRC | volume of air in lungs after a normal tidal respiration (FRC=reserve volume + expiratory reserve volume) |
| Total Lung Capacity TLC | volume in lungs after maximal inspiration |
| FEV1 | volume exhaled in first second of an FVC |
| FET Forced Expiratory Time | Time taken for subject to exhale their vital capacity in a forced expiration (3-4 secs) |
| Maximum Mid Expiratory Flow MMEF | the flow rate of expired air over the middle 50% of the FVC |
| Maximum Voluntary Ventilation MVV | max volume of air that can be moved in and out of the lung per unit |
| Vital Capacity VC | Total volume expelled by a slow exhalation from a maximal inspiration |
| Residual Volume RV | |
| Spirometry patterns – obstructive and restrictive lung disease | |
|---|---|
| normal | Sharp bend or knee at around 1 second as flow reduces and lung empties.Ratio of FEV1 to FVC should be > 0.7 |
| obstructive | FEV1/FVC <80%increased TLC increased FRC increased RVAsthma COPD Empysema Bronchiectasis |
| restrictive |
|
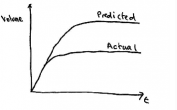
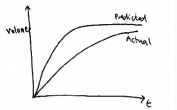
Spirometry volume flow loop
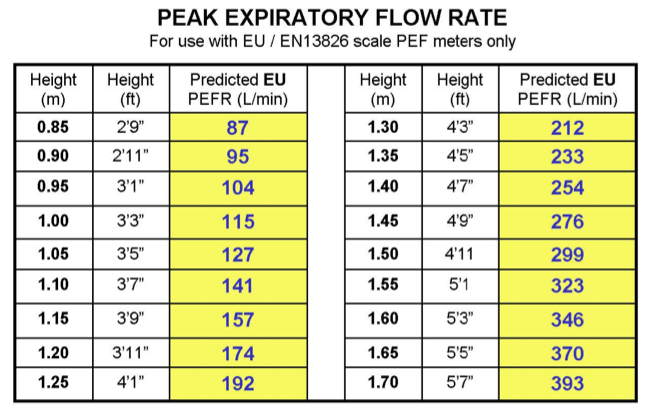
Peak flow meters
http://www.youtube.com/watch?v=LPA-XKU3hD8
http://www.youtube.com/watch?v=dPDHsReZfQ0
www.peakflow.com.
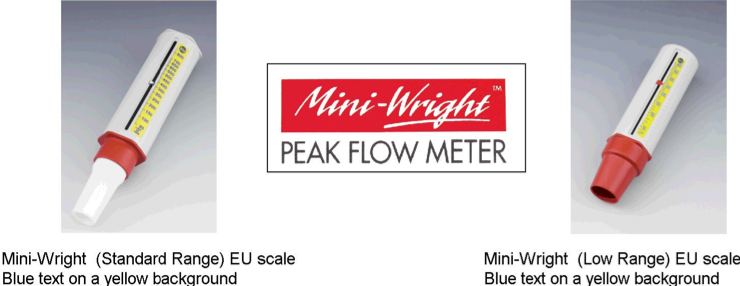
- Peak flow measurement
- Set meter to zero
- Connect disposable mouthpiece
- Stand (or if unable sit) upright
- Make sure fingers do not obstruct the PEFR slide
- Inhale deeply, place lips around meter making a tight seal. Breathe out forecfully whilst holding the meter horizontal.
- Note the reading
- Repeat twice unless patient unable to do so
- Record the highest of the 3 readings.
Asthma
Acute Asthma – see emergencies section
Episodic variable airways obstruction characterised by
- 1 hyper-reactivity and hypertrophy of bronchiolar smooth muscle
- 2 chronic inflammation and oedema of bronchiolar walls and
- 3 excessive secretion of thick mucus which plugs the bronchioles and narrows the airways still further
Symptoms may be triggered by exercise, change in temperature, smoky environments and be worse at night. May be history of atopy.
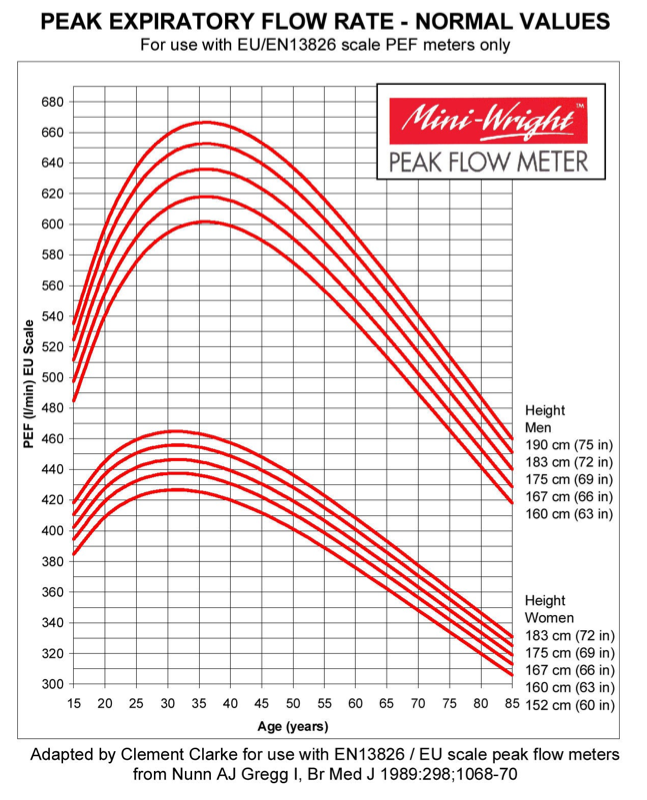
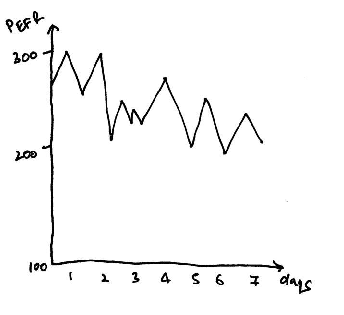
Diagnosis is suspected clinically based on symptoms but must be confirmed by spirometry, demonstration of pef variability and response to treatment.
- http://www.youtube.com/watch?v=82gn_rDRpHk
- http://www.youtube.com/watch?v=vlZ7R07OrR4
- http://www.asthma.org.uk
Asthma pathophysiology
- http://youtu.be/7EDo9pUYvPE
- http://youtu.be/Zlnsx8zKLvQ
- http://youtu.be/v-qr78Wj4xM
- Asthma pathophysiology @ Emedicine
- slideshare.net Asthma pathophysiology
Diurnal variability
- Worse at night and early morning best in afternoon.
- % variability = (highest- lowest reading)/highest reading x 100
- Asthma likely if
- PEF variabilty > 20%
- > 60 l/min
- Occurs > 3days over 2 week monitoring period
Asthma treatments
| Short and long acting Beta agonists | |
|---|---|
SABA
|
1 Cause relaxation of bronchiolar smooth muscleonset 10m peak 25m duration 4-6 hrs2 Inhibit release of inflammatory mediation3 Improve clearance of mucusUsed for acute relief or in anticipation of bronchospasm eg before exercise.Nebulised salbutamol 2.5-5mg every 15-30m in severe asthma. |
LABA
|
Relieve symptoms over 12hr periodSide-effects – tremor, nervous tension hypokalaemia and muscle crampsLABA must never be used in asthma without an inhaled corticosteroid – risk of severe acute asthma and death |
Inhaled steroidsmainstay of treatment in asthma |
|
|---|---|
| Actions |
|
| Side Effects |
At lower doses little steroid is absorbed systemically side-effects are minimal even in children. Higher doses of inhaled steroids and oral steroids may cause adrenal suppression. |
| Local | Sore mouth, hoarse voice and oropharyngeal thrush infection due to local immune suppression.Reduce by using a spacer or by rinsing mouth and throat after use. |
| Systemic | During long-term use of high dose inhaled (or oral steroids) there may be increased risk of osteoporosis in adults, and the dose of steroid should be kept at the lowest level needed to control symptomsExcessive doses should be avoided in children, due to the risk of significant systemic absorption and adrenal suppression. |
| Preparations |
|
3rd/4th line treatments
| Leukotriene receptor blockers – montelukast zafirlukast |
|---|
| Block inflammatory mediators released by eosinophils and other inflammatory cells which would otherwise cause bronchoconstriction, increased mucus secretion and mucosal oedema.Effective especially in exercise induced asthma and rhinitis associated asthmaod oral ingestionSide effects: GI disturbance, headache, thirst, insomnia |
| Short acting Antimuscarinics – Ipratropium |
|---|
|
| Long acting anticholinergic Tiotropium used in COPD only |
| Block acetylcholine from the vagal parasympathetic fibres reducing bronchoconstriction and mucus secretionside effects: dry mouth, nausea, constipation, glaucoma bladder outflow obstruction tachycardia |
| Xanthines Theophylline Aminophylline |
|---|
| Phosphodiesterase inhibitorsCause build up of cAMP relaxing airway smooth muscleUsed in stable COPD or acute severe asthma |
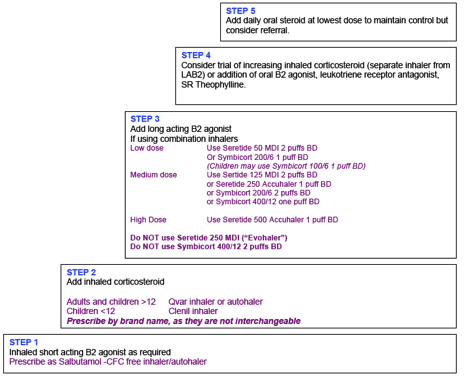
| Asthma guidelines Adults SIGN/BTS 2011 | |
|---|---|
| 1 mild intermittent |
short acting β-agonist prn |
| 2 regular preventer |
add inhaled steroid200-800 μg BDP equivalent/day |
| 3 add-on therapy |
add LABAonly continue if good responseotherwise increase steroid to 800 μg/d |
| 4 persistant poor control |
Increase steroid to 2000 μg/d consider adding other Rx:leukotriene antagonistsor β-agonist tabsor SR theophylline |
| 5 frequent continuous oral steroids |
Refer |
Single maintenance and reliever therapy SMART
eg Symbicort (budesonide/formoterol) can be used for maintenance therapy and the dose temporarily increased to provide relief of exacerbations – simplifying management and reducing prescription cost to patients. SMART DTB Nov 2011
Poor control
- Use of > two B2 agonist MDIs per month
- Use of a B2 agonist 3x/week or more
- Nocturnal symptoms, daytime symptoms, limitation of normal activity
| Asthma guidelines children under 5 | |
|---|---|
| 1 mild intermittent | short acting β-agonist prn |
| 2 regular preventer | add inhaled steroid200-400 μg/d in bd doseconsider LRA if inhaled steroid can’t be used |
| 3 add-on therapy | add long acting β-agonistConsider adding leukotriene receptor antagonists.In those children already taking leukotriene antagonists alone reconsider adding steroid 200-400mcg/dayIn children under 2 years consider going to Step 4 |
| 4 persistant poor control | refer paeds |
| Asthma children 5-12 SIGN/BTS 2011 | |
|---|---|
| 1 mild intermittent | short acting B2 agonist prn |
| 2 regular preventer | add inhaled steroid 200-400μg/dor leukotrine antagonist if steroids cant be usedstart at 200μg/d in two divided doses |
| 3 add-on therapy | inhaled steroids 200-400 μg/dayadd LABA |
| 4 persistant poor control | inhaled steroid 400 μg/dinhaled LABAconsider trials of increased steroids to 400 μg/d and referralcontinue LABA increase steroids if still poor controlbut stop LABA if no response to thisConsider leukotrine antagonist or theophylline |
| 5 high dose/oral steroids | inhaled steroid 800 μg/d oral steroids at lowest doserefer paeds |
| Inhaled asthma drugs | |
|---|---|
| Anti-inflammatory | Sodium Chromoglycate = Intal or Nedocromil =Tilade |
| SA anticholinergic | Ipratropium = Atrovent |
| LA anticholinergic Tiatropium/Spiriva COPD only | |
| Steroids | Beclomethasone = Qvar Asmabec Pulvinal ClenilBudesonide = PulmicortFluticosone = FlixotideMometasone=Asmanex |
| SABA | Salbutamol = Ventolin Salamol AsmasalTerbutaline = Bricanyl |
| LABA | Salmeterol = Serevent NeoventBambuterol = BambuterolFormoterol = Oxis Atimos |
| Combinations | |
|---|---|
| Combivent | ipratropium+salbutamol |
| Symbicort | 100/6 Budesonide+Formoterol |
| Fostair | Beclomethasone+Formoterol |
| Seretide | Fluticasone+Salmeterol |
| seretide like flixotide serevent like ventolin | |
|---|---|
| salbutamol | ventolin |
| salmeterol | serevent |
| seretide | serevent + flixotide |
| Seretide accuhaler | salmeterol 50mcg+ flixotide (100/250/500) |
| Seretide evohaler | salmeterol 25mcg+ flixotide (50/125/250) |
- Shake inhaler
- Remove cap
- Inhale deeply then fully exhale
- Seal mouth lips around mouthpiece
- Breathe in via mouthpiece whilst pressing down on top of inhaler
- Continue breathing in deeply to get drug deep into lungs
- Hold breathe for 10 seconds or as long as is comfortable, then breathe out slowly
- Repeat as necessary after 30 seconds
- Replace cap on mouthpiece
- If steroid inhaler rinse out mouth.
GOLD guide inhalers and spacers
| Spacer devices | |
|---|---|
| volumatic | salbutamol salmeterol fluticasone beclomethasone seretide |
| aerochamber | salbutamol terbutaline salmeterol fluticasone beclomethasone budesonide seretide symbicort atrovent |
| able spacer | salbutamol terbutaline salmeterol fluticasone beclonethasone budesonide seretide symbicort atrovent |
| nebuhaler | terbutaline budesonide symbicort atrovent |
Spacers
- An MDI & spacer is the preferred option in adults and should be used in all < 12s.
- Advantages – greater delivery to the bronchioles, less oral deposition, so reduced frequency of oral thrush and it is as good as a nebuliser during acute exacerbations.
- Should be demonstrated and technique checked.
- Should be washed weekly with detergent and allowed to air dry (NOT wiped dry).
- Should be changed every six months.
- Inspiration should take place as soon as possible after MDI actuation.
- Tidal breathing (x5) is as effective as and more preferable than deep breathing.
http://www.youtube.com/watch?v=CEUm–zy8xY
http://www.youtube.com/watch?v=8BaT2XIrePE
http://www.youtube.com/watch?v=h6eD81NyBAU
http://www.youtube.com/watch?v=esmEVr4qROQ
http://www.youtube.com/watch?v=A7DhGX0p1KY
Inhalers and choice of device
MIMS Chart – asthma & COPD preperationss and devices
MDI
MDI and spacer
Autohaler – Easibreather breath actuated inhaler
DPI / turbohaler
Accuhaler
| Inhaler | Colour / appearance |
|---|---|
| SABA | blue |
| SA antimuscarinic | grey or clear + green |
| LABA | green |
| LA antimuscarinic | oval container requiting capsules |
| Steroid | brown /maroonorange (fluticasone) |
| Combined steroid / LABA | Purple or red |
Asthma monitoring and review |
|---|
| Patient understanding of ‘preventers’ and ‘relievers’ and their appropriate usage, also ask about any side effects. |
| inhaler technique. |
| Compliance as per computer and patient history – number of salbutamol MDIs used |
| Any exacerbations, hospital admissions or oral steroid use since last review |
RCP 3 Questions
|
| Other markers of controlHaving to use a reliever more than 3 x per week? |
| The need to step up or step down treatment ? change self management planIf symptoms control excellent over a period of at least three months then consider dropping the inhaled steroid dose by 25 to 50% and review after another three months. |
| Check Smoking status and cessation advice. |
| Osteoporosis risk Adults who have used oral steroids for > 3 months or have had 3 or more courses of oral steroids in a life time need a DEXA scan and consideration for osteoporosis prophylaxis e.g. biphosphonates. Furthermore, patients on beclomethasone doses greater than 800mcg a day should be considered for osteoporosis prevention lifestyle advice +/Calcichew D3 forte. |
At repeat medication re-authorisation clinician should look at
|
| Check Smoking status and cessation advice |
Asthma (Read Code H33)
Clinical features that increase the probability of asthma
Diagnosis (adults) – base initial diagnosis on a careful assessment of symptoms and spirometry (or PFR if unavailable, see below). Move straight to a trial of treatment if a high probability of asthma.
Note: PFR based diagnosis may be used in a Primary care setting.
>20% diurnal variation in recorded EU PFR (am and pm prior to any beta agonists) on 3 or more days each week for 2 weeks.
Variation % = (maximum PFR-minimum PFR)/ maximum PFR x100.
Diagnosis (children) – assess clinically with symptoms (see below). Move straight to a trial of treatment if high probability of asthma. If less clear, consider lung function tests, if age >5 (spirometry pre and post bronchodilator, PFR).
Do not add children to the asthma register unless you are confident of the diagnosis!
Clinical features that increase the probability of asthma
-
More than one of the following symptoms: wheeze, breathlessness,
chest tightness and cough, particularly if:
- Symptoms worse at night and in the early morning
- Symptoms in response to exercise, allergen exposure and cold air
- Symptoms after taking aspirin or beta blockers
-
History of atopic disorder
- Family history of asthma and/or atopic disorder
-
Widespread wheeze heard on auscultation of the chest
- Otherwise unexplained low FEV1 or PEF (historical or serial readings)
Otherwise unexplained peripheral blood eosinophilia
Spirometry based diagnosis (may be falsely negative in a patient who is well at time of assessment)
Fev1/FVC < 70% = an obstructive picture (Asthma or COPD) but in asthma there is reversibility in the lung function.
>15% or > 200mls improvement in FEV1 after 400mcg (4 puffs via an MDI) of salbutamol via a volumatic.
>15% or > 200mls deterioration in FEV1 after 15mins of exercise.
- Having made the diagnosis please place them on the asthma register and put the H33 Asthma Read code in their Problem page.
-
Arrange a New Patient Asthma clinic appointment with the Practice Nurse.
Don’t forget basic health promotion!
-
Smoking status and cessation advice – Read code.
-
Flu vaccination if on inhaled steroids
-
Life style and exercise.
-
Asthma self management plan.
-
Patient information leaflets.
- Pre-payment certificates for script costs.
Adult asthma guidelines BTS 2011
Step 1 Inhaled short acting B2 agonist as required
Step 2 Add inhaled steroid 200-800mcg BDP equivalent/day bearing in mind that 400mcg is the starting dose for many patients
Step 3 Add inhaled Long Acting B2 agonist (LABA) .
-
Continue LABA if there is a good response
-
Discontinue LABA if no response and increase inhaled steroid to 800mcg a day
- If some benefit from LABA but control inadequate increase inhaled steroids to 800mcg/day and then consider adding in other therapies e.g. leukotriene receptor antagonists (1 month trial) or SR theophylline.
Step 4 Consider trials of:
-
Increased inhaled steroid up to 2000mcg a day.
- 4th drug. Eg. Leukotriene receptor antagonist, B2 agonist tablets or theophylline.
Step 5 Consider:
-
Oral steroid at lowest dose to maintain control
-
Maintain high dose inhaled steroid 2000 mcg/day
-
Other treatments to minimize oral steroid use.
Refer.
Note: start at the step most appropriate to initial severity. Step up (remember check concordance and diagnosis) or step down depending on control.
Indications to progress to a higher step.
Usage of > one B2 agonist MDI per month = poor control.
Usage of a B2 agonist 3x/week or more = poor control.
Nocturnal symptoms, daytime symptoms, limitation of normal activity = poor control
Please note the preferred CFC free beclomethasone inhaler is Clenil Modulite (should be prescribed as brand) and is dose for dose equivalent to Becotide. Avoid QVAR which is expensive and not bio equivalent to Becotide.
Children 5-12 years asthma guidelines BTS 2011
Step 1 Inhaled short acting B2 agonist as required
Step 2 Add inhaled steroid 200-400mcg BDP equivalent/day bearing in mind that 200mcg is the starting dose for many patients (but dose appropriate to severity of disease)
Step 3 Add inhaled Long Acting B2 agonist (LABA) .
-
Continue LABA if there is a good response
-
Discontinue LABA if no response and increase inhaled steroid to 400mcg a day
- If some benefit from LABA but control inadequate increase inhaled steroids to 400mcg/day.
- Consider adding in other therapies e.g. leukotriene receptor antgonists or SR theophylline.
Step 4 Increase inhaled steroid up to 800mcg a day.
Step 5 Consider:
-
Use daily steroid tablet in lowest dose possible to maintain control.
-
Continue high dose inhaled steroid 800mcg a day
Refer.
Children under 5 years BTS asthma guidelines 2011
Step 1 Inhaled short acting B2 agonist as required
Step 2 Add inhaled steroid 200-400mcg BDP equivalent/day bearing in mind that 200mcg is the starting dose for many patients (but dose appopropriate to severity of disease) or leukotriene receptor antagonist if inhaled steroid can’t be used.
Step 3 Children < 2 years consider going to step 4.
Children > 2 years:
-
In those taking inhaled steroids 200-400mcg/day consider adding leukotriene receptor antagonists.
- In those taking leukotriene receptor antagonists alone reconsider the addition of inhaled steroid 200-400mcg/day.
Step 4 Refer
Note: monitor growth in children.
Factors to assess on asthma/medication review – 10 points!
-
Patient understanding of ‘preventers’ and ‘relievers’ and their appropriate usage, also ask about any side effects.
- Check inhaler & spacer technique.
- Compliance as per computer and patient history – number of salbutamol MDIs used in last 12 months
-
Have they had a new spacer within the last 12 months?
-
Smoking status and cessation advice.
- Any exacerbations, hospital admissions or oral steroid use since last review?
- The RCP 3 Questions
-
Has your asthma interfered with your usual activities (e.g. housework, work, school, hobbies etc)?
- Have you had difficulties sleeping because of your asthma symptoms (including cough)?
-
Have you had your usual asthma symptoms during the day (cough, wheeze, chest tightness or breathlessness?)
-
Having to use a reliever more than 3 x per week?
- The need to step up or step down treatment – ? change self management plan.*
-
Are they aware of the month of their next annual review (schedule of care)?
*Review should incorporate a written action plan (BTS 2011). Download the ‘Be in Control’ asthma action plan ( or ‘My Asthma for age 6-11) from www.asthma.org.uk/control .
Osteoporosis risk
Treatment strategy for preventing steroid induced osteoporosis
Consider every patient for active osteoporosis prevention who has had:
- Oral or iv steroid treatment for greater than 3 months.
- A cumulative lifetime dose of 1g oral prednisolone (e.g. > 4 x seven day courses in a lifetime).
- Inhaled steroid > 1000mcg day beclomethasone.
If unable to have a DEXA then treat, 1st line = a bisphosphonate.
If steroid course likely to > 3 months then treat, 1st line = a bisphosphonate.
If able to have a DEXA and the T score above -1.5 treat with lifestyle measures +/- calcium supplementation.
NB DEXA needs repeating every 3 years
If the T score is = -1.5 or lower then treat, 1st line = a bisphosphonate.
NB DEXA needs repeating every 3 years
Indication for consultant referral
-
Diagnosis unclear.
-
Failure to control symptoms beyond Step 4.
-
Consideration for home nebs or home oxygen.
-
Acute severe exacerbations.
-
Troublesome drug side effects or complications of Rx/asthma.
-
Suspected occupational asthma
Structure of the asthma service
All patients with proven asthma will be tagged with the H33 Read code, as this is required for Read code QOF based recall which identifies patients who have not had a formal asthma review in the last 15 months.
At repeat medication re-authorisation doctors must look at:
- Beta 2 agonist over usage – arrange GP review?
-
Spacer on repeat script? Check when last issued.
-
Oral steroid/high dose inhaled steroid usage and need for osteoporosis prophylaxis.
- Correct Read H33 Read coding & is it in the Problem page?
- Annual review in date?
- If seeing the patient for their annual review ask and document the ten point review ( use S1 template along with prompts from the auto-consultation).
QOF 2011/12
Asthma 3 – Annual recording of smoking status in asthmatic patients ages 14-19.
Target 80%.
Asthma 6 – Annual asthma review to be recorded.
Target 70%.
Asthma 8 – Post 1/4/06 need to record ‘measures of variability or reversibility’ at
diagnosis of patients aged 8 and over.
Target 80%.
References: British Guideline on the Management of Asthma – BTS.
May 2011.
QOF.
Indication for consultant referral
- Diagnosis unclear.
- Failure to control symptoms beyond Step 4.
- Consideration for home nebs or home oxygen.
- Acute severe exacerbations.
- Troublesome drug side effects or complications of Rx/asthma.
- Suspected occupational asthma
Asthma management plans
Asthma in adults: Creating an asthma action plan Mayo Clinic
Asthma control test adults and children
Drugs causing asthma |
|
|---|---|
| AspirinNSAIDs | Cyclo-oxygenase inhibitors which reduce the production of bronchodilating prostaglandins.Asthmatics should be repeatedly warned to avoid aspirin and all NSAIDs |
| Beta Blockers | Block the bronchodilating beta2-receptors in the bronchioles, precipitating asthma in predisposed patients also prevent access by salbutamol and terbutaline to the bronchiolar beta-receptors should acute attack occur.All beta-blockers may precipitate acute asthma in predisposed patients, even in minute doses (e.g. eye drops).Selective beta-blockers are safer but should still be avoided if possible |
| N-Acetyl cysteine | used to treat paracetamol toxicity |
| Tartrazine | food colourant/additive |
| webmd.com medications triggering asthma | |
Asthma allergies and rhinitis
There is an overlap between asthma and atopic conditions such as eczema and allergic rhinitis.
Patients may have raised IgE and eosinophils and may test positive on RAST or patch testing.
Treatment of allergic rhinitis will improve asthma control.
Asthma and rhinitis are type 1 (immediate) hypersensitivity reactions – inhaled antigens bind to IgE on surface o mast cells causing degranulation and release of inflammatory mediators. Symptoms can come on over 5-10 min.
Asthma and Allergic Rhinitis Questionnaire allergy uk.org
Allergy Testing
Allergen avoidance
Grass and fungal pollens
Housedust mites
Pets
Occupational
Asthma prevention
Breastfeeding may have protective effect on child, and so should be encouraged due to other beneficial effects.
Breathing exercises
COPD
Chronic slowly progressive lung disease of smokers.
Obstructive pattern on spirometry.
Degree of impairement is relatively stable over period of months (without diurnal or day to day variability).
Airflow obstruction is partially/minimally reversible by bronchodilator or other therapy.
- COPD
- Characteristic signs and symptoms plus an obstructive spirometry with post-bronchodilator FEV1/FVC ratio of 0.7.
- FEV1 < 80% predicted
- FEV1/FEV ratio < 70 % (ie obstructive picture)
- no diurnal variation and little <15% or 200mls reversibility.
| COPD previously classified into 2 clinico-pathological syndromes | |
|---|---|
| chronic bronchitis | daily cough productive of sputum for 3 months in 2 consequitive years. |
| emphysema | destruction of alveolar walls causing irreversible expansion and air trapping. |
| Severity | FEV1 | Clinically |
|---|---|---|
| mild | 50–80%predicted | Chronic cough with SOB on maximal moderate exertion |
| moderate | 30–49%predicted | Chronic cough with SOB on minimal exercise+/- cor pulmonale |
| severe | < 30%predicted | SOB at rest and severe limitation of exercise |
COPD diagnosis
Hx > 10 pack years smoking hx and > 35 years – if not reconsider the diagnosis.
FEV1/FEV ratio <70%, with no significant reversibility
Grade and record mild, moderate or severe on the basis of Fev1/predicted.
CXR to exclude bullae, tumour, pulmonary oedema, bronchiectasis etc.
FBC if suspicion of anaemia or polycyctheamia.
| MRC breathless scale | |
|---|---|
| 1 | Not troubled by breathlessness except on strenuous exercise |
| 2 | Short of breath when hurrying or walking up a slight hill |
| 3 | Walks slower than contemporaries on level ground because of breathing or has to stop for breath when walking at own pace |
| 4 | Stops for breath after walking about 100m or after few minutes on level ground |
| 5 | Too breathless to leave the house, or breathless when dressing/undressing |
COPD management
Nonpharmacological
- Smoking cessation is the most important intervention and will slow further decline to the rate of a non-smoker (see Pareto graph)
- Pulmonary rehabilitation should be offered to all patients who are functionally limited by COPD, (MRC Grade 3 and above) including those who have had a recent hospitalisation or exacerbation. Pulmonary rehabilitation is not suitable for patients who are unable to walk or who have had a recent MI. Polmonary rehab invimvolves a 6-12 w program of exrercise, education psychological and social interventions delivered by MDTs of respiratory physiotherapists and nurse.
- Explanation and information about COPD for patient and carers.
- Flu & Pneumovax vaccination.
- Increasing exercise +/ weight loss increase lung function and decrease symptom scoring.
- Screen for and treat depression, which is often missed by doctors.
- Met. Office Health Forecasting – early warning and telephone support for patients
- Winter fuel programmes
- Work with the patient to develop a self management plan:
- When to seek an antibiotic.
- When to seek oral steroids.
- When to seek medical advice.
- When to seek emergency medical advice.
COPD medical management |
|
|---|---|
| Airflow obstruction in COPD is mostly irreversible but bronchodilatiors can help to some degree. | |
| Mucolytics | trial of carbocisteine for four weeks if chronic productive coughavoid if they history of peptic ulcerStop if no improvement |
| Short Acting Bronchodilators |
antimuscarinics preferered to SABA in COPD as they reduce mucus hypersecretion as well as causing bronchodilation |
| Long Acting Bronchodilators |
antimuscarinics (tiotropium) or LABA (salmeterol eformoterol)if tiotropium started then stop ipratropium.LABAs are usually prescribed with a steroid though it is not clear if there is the same risk as when used alone in asthmaCOPD (Spiriva) |
| Short + Long acting bronchodilators |
if not already on Symbicort/Seretide for exacerbation prevention – see below |
| Steroids | have little effect in COPD.May slightly improve FEV1 at high dose and reduce exacerbations.Hence reserved for psatients with FEV1 <50% and > 2 exacerbations per year.usually given as LABA/ steroid combination eg Seretide 500 1 puff BD. |
| Xanthines | may be worth trying in patients unresponsive to the above |
When to refer
- Uncertain diagnosis e.g. Hx or Ex = age <35, < 10 pack years, wt loss, haemoptysis etc, unilateral signs.
- Atypical spirometry – restrictive rather than an obstructive picture.
- Failure to respond to Rx. Check compliance and technique first
- Consideration for oral steroids long term, home nebs or LTOT
- Complications, such as Cor Pulmonale
- Severe COPD.
- surgery bullectomy, lung transplant, lung volume reduction surgery
Refer for LTOT if
- FEV< 30%
- Cyanosis
- Polycythemia
- Cor pulmonale
- Peripheral oedema
- O2 sats <92% in room air.
Consider Palliative care if 2 or more of following consistently
- FEV1 <30% of predicted
- SOB on any exertion
- Significant wt loss
- Recurrent admissions for exacerbations
- Social isolation/depression
- Severe heart failure
COPD inhalers
LABAs in COPD and asthma
Controversies Regarding Long-acting ?2-agonists Medscape
http://www.pamf.org/asthma/medications/inhaled/longacting.html
Mucolytics in COPD
Oxygen in COPD
http://hacking-medschool.com/oxygen-prescription-domicilliary-oxygen
Exacerbations COPD
1 Increased sputum volume or discoloured sputum use antibiotics for 1 week (amoxycllin or erythromycin 1st line).
30% are viral, 30-50% bacterial in origin with the remainder undetermined.
Prescribe antibiotics if increased sputum purulence.
If no increase in sputum purulence then antibiotics are not needed unless consolidation on chest x-ray or other signs of pneumonia.
Organism H.influenzae, S.pneumoniae, M.catarrhalis.
Rx Amoxicillin 500mg three times daily for five days, or doxycycline 200mg Day 1 then 100mg daily for 4 days.
Co-amoxiclav or ciprofloxacin 2nd line for 1 week if no improvement
2 SOB/wheeze – increase salbutamol use to at least QDS via a spacer.
3 Consider oral steroids (prednisolone 40mg a day for 7 to 10 days) if
a) are known to be steroid responsive
b) a new presentation where steroid responsiveness in unknown or
c) are already on steroids.
Remember they need a DEXA scan and consideration for osteoporosis prophylaxis if they have more than 3 months of oral steroids or 3 courses on oral steroids in a 12month period.
Indications for admission
Admit to hospital if unwell (e.g. confused, cyanosed, very short of breath), no improvement on treatment, unable to cope at home
- Signs of a severe acute exacerbation = cyanosis, RR > 25, Pulse > 110, unable to speak in sentences or confused.
- Patient already on maximum treatment
- Patient on LTOT
- Patient unable to cope at home
- Failure to respond to Rx
- Complications e.g. Cor pulmonal
| COPD Home Versus Hospital (NICE 2004 EFIGM 2005) | ||
|---|---|---|
| factor | favours hospital Rx | favours home rx |
| able to manage at home | no | yes |
| breathlessness | severe | mild |
| general condition | poor/deteriorating | good |
| level of activity | poor/bed-bound | good |
| cyanosis | yes | no |
| worsening oedema | yes | no |
| concious level | impaired | normal |
| already on LTOT | yes | no |
| social circumstances | living alone / not coping | good |
| acute confusion | yes | no |
| rapid rate onset | yes | no |
| significant comorbidity | yes | no |
| SaO2<90% | yes | no |
| CXR changes | yes | no |
| arterial pH | <7.35 | >7.35 |
| arterial pO2 | <7kPa | >7kPa |
COPD patient letter
We are writing with some important information for you about your COPD (also known as chronic bronchitis and emphysema)
Many people with COPD get flare ups of their condition (sometimes called chest infections or exacerbations). Flare ups happen much more frequently in the winter months, particularly if the weather is very cold. This increase in flare ups leads to increased pressure on emergency services, hospitals and A&E departments. However we know that if you can recognise a flare up early and take the correct action you can avoid A&E and reduce your risk of a hospital admission.
Reducing your risk of flare ups and hospital admissions
Make sure you have at least a week’s supply of your regular medicines throughout the winter.
Keep your house warm. The living area should be around 21 degrees and the bedroom 18 degrees. If you would like help with keeping your house warm contact AWARM on 245 7422.
Recognise the early signs of a flare up:
- More breathless than usual
- More phlegm than usual
- Your phlegm changes colour
If you think you are experiencing a flare up contact your GP or practice nurse as soon as possible for advice.
If you already have a self management action plan use your rescue medications as soon as you notice a flare up starting.
You can also contact NHS Direct on 0845 4647 for advice if you are unsure about your symptoms or your medications.
If you are known to the CAST team, you can ring them directly on their number that you will have been supplied with previously. If they are not available to take your call leave a short clear message on the answer phone with your name and contact details. They will get back to you within 24 hours.
Please only attend the A&E Department at the Hospital if you are unwell and your condition can’t wait or if you have accessed all of the above without improvement. Remember that A&E services are for major injuries and life threatening illness only.
Remember to keep warm, keep well and choose well this winter.
(Salford NHS)
COPD self management plan
KNOW YOUR MEDICATION
INHALERS
Bronchodilators (Relievers): These relax the muscles in your airways & make it easier for you to breathe. Shorting acting inhalers start to work within about 10 minutes & the effect should last about 4 hours. Your short acting ‘reliever’ medication is ______________________
Long acting inhalers (Preventers) take longer to take effect but last 12 –24 hours.
Your long acting medications are__________________
Steroid inhalers (Preventers): usually used with a spacer device. They are often combined in a single inhaler with one of the long acting bronchodilators.
Your steroid inhaler is _____________
Please contact your surgery in plenty of time to ensure you don’t run out of any of your medication
EXACERBATIONS (when you get worse)
You should increase your treatment early when you are unwell. You should have a ready supply at home of additional tablet medications needed if you are feeling worse (eg antibiotics, steroids). If you are unwell, follow the instructions on page 3 of this leaflet.
ADDITIONAL TABLET MEDICATIONS.
These tablet medications may be prescribed to help your breathing.
Steroid Tablets (Prednisolone 5mg): A course of these may need to be taken during an exacerbation and are taken in one morning dose.
Steroid tablet instructions: _________________________
Antibiotics: These should be taken if you have symptoms of infection ie coloured phlegm, increased phlegm being coughed up.
Antibiotic instructions: ______________________________
COPD Review
http://hacking-medschool.com/qof-copd
Hospital at home
Pulmonary Rehabilitation @ medscape
BTS Pulmonary Rehab Guidelines
Alpha 1 antitrypsin deficiency
A1 antitrypsin breaks down neutrophil elastase in the lung. Congenital deficiency (Autosomal Codominant) allows the latter to run amok breaking down lung parenchymal tissue causing COPD and emphysema at an earlier age in smokers and nonsmokers.
Alpha 1 antitrypsin defficiency Medscape
| Respiratory failure definition | |
|---|---|
| Arterial PaO2 <8kPa (normal range 10-13.1 kPa) | |
| type 1 | PaO2 <8kPa no hypercapnia |
| type 2 | PaO2 <8kPa plus hypercapnia |
| Respiratory failure aetiology | |
|---|---|
| Type1 | impaired gas transfer across alveolar capillary membranedue to loss of alveolar tissue or increased thickness of alveolar capillary membraneDiffusion coefficient CO2 is 20 times that of O2 so this not affected unless/until gas transfer severely affected |
| Type2 | reduced PaO2 and CO2 accumulationdue to hypoventilation (see below)or severe lung disease affecting exchange of both O2 and CO2end stage COPD, status asthmaticus, massive PE |
| Causes of hypoventilation | |
|---|---|
| Central |
|
| Neurological |
|
| Chest wall deformity |
|
Pink Puffers and Blue Bloaters
Respiratory failure scottishintensivecare.org.uk
Domicilliary oxygen |
|
|---|---|
| Intermittent | as required use for intermittent symptom controlif >21 cylinders/month then concentrator may be more economicalmay be sometimes appropriate in terminal care but O2 not indicated for simple breathlessness |
| LTOT | Patients with chronic respiratory failure who1) they do not smoke; and2) they have a PaO2 < 7.3 kPa whilst breathing room air during a period of stability at least one month after any exacerbation of their lung disease. COPD patients who continue to smoke do not derive the improved survival benefits of LTOT.Patients with COPD will only derive benefit if oxygen therapy is used for at least 15 hours/day.For patients with COPD 2l/min via nasal prongs is standard therapy, however higher rates of flow may be required, as guided by the respiratory physiciansPatients with type 1 respiratory failure may require significantly higher rates of flow, and subsequently need multiple oxygen concentrators |
| Ambulatory | patients who desaturate on exercisePortable oxygen cylinders are available on a GP prescription(DD and PD size lightweight cylinder)following evaluation by a respiratory physician |
Prescribe on HOOF form and fax directy to supplier (dependant on local arrangements/contracts) who then deliver directly to patients home.
MIMS Oxygen Concentrators: Procedure for Prescribing Tables
Oxygen is a drug and should therefore be prescribed. Inappropriate concentrations may have serious or even lethal effects.
Patients should be advised of the fire risks with oxygen and they or their contacts must not smoke in the same environment.
Oxygen can be delivered either nasally or by mask. Prescribers should specify the oxygen delivery percentage, and flow rate for the mask, and the flow rate for nasal delivery.
The administration of high oxygen concentrations in acute COPD and other conditions vulnerable to hypercapnic respiratory failure leads to worsening of hypercapnic respiratory failure and respiratory acidosis. Patients with COPD (and other at-risk conditions) who have had an episode of hypercapnic respiratory failure should be issued with an oxygen alert card and a 24% or 28% Venturi mask. They should be instructed to show the card to the ambulance crew and emergency department staff in the event of an exacerbation. Alert cards are issued by the respiratory liaison nurse during a hospital admission.
Acute Respiratory Failure
Acute respiratory failure Nursing Times.net
ARDS
Adult Respiratory Distress Syndrome
Obstructive sleep apnoea
Sign 73 OSAHS – obstructive sleep apnoea/hypopnoea syndrome
Due to repeated intermittent upper airway colapse during sleep causing total obstruction (apnoea – patient stops breathing) or partial obstruction with (hypoventilation / hypoapnoea and snoring)
Patient goes through cycle of deep sleep with airways collase then stimulation /arousal with increased inspiratory effort and restoration of muscle tone then deeper sleep again.
Causes daytime sleepiness and increased CVS risk (via increased BP and as indipendant risk factor)
britishsnoring.co.uk epworth scale
Diagnosis is confirmed by sleep studies involving measurement of pulse oximetry, nasal airflow, snoring and respiratory effort.
Treatment
Behavioural
Wt loss, smoking, alcohol, eelevation of bed, avoid sleeping on back.
CPAP
Positive pressure from nasal or face mask splints open the upper airways preventing collapse and apnoea during deep sleep. Used for moderate (30-50) and severe (>50 apnoea/hypoapnoeas per hr) sleep apnoea.
Mandibular Advancement devices
Dental appliances which pull the jaw forward increasing airway diameter. Used in mild sleep apnoea or in patients intolerant of CPAP
| URTI MRTI LRTI | |
|---|---|
| URTI | rhinitisotitissinusitistonsillitsmastoiditispharyngitis |
| MRTI | laryngitislaryngotracheitisepiglottitisbronchitis |
| LRTI | pneumoniabronchiolitisempyema |
Antibiotics in URTI
http://hacking-medschool.com/antibiotic-resistance
Delayed antibiotic prescriptions
Delayed Antibiotic Prescriptions cfp.ca
Common cold
Pharyngitis laryngitis tonsilitis
medical center.osu.edu tonsils
Peritonsilar Abcess Quinsy
http://hacking-medschool.com/quinsy-peritonsillar-abcess
Acute bronchitis and cough
Acute bronchitis and cough MeReC 2006;17(3)
Average length of illness is 3 weeks.
Most are viral and use of antibiotics have little benefit in otherwise healthy adults.
More benefit if > 65 years with cough and other co-morbidities.
Organism H.influenzae, S.pneumoniae, M.catarrhalis.
Treatment Amoxicillin 500mg three times daily for five days, or doxycycline 200mg Day 1 then 100mg daily for 4 days.
Cough causes
- Pulmonary – any lung disease, asthma, smoking
- Nasal – rhinosinusitis with post nasal drip
- Oesophageal – GORD
- Drugs – ACEIs
Safety net Refer urgently if potential cancer (under 2 week rule)
Acute cough has a sudden onset and usually lasts less than 3 weeks. Chronic cough lasts longer than three weeks.
Bronchitis- Is an inflammatory disorder that is usually caused by a virus; it can be acute or chronic in nature. Common offenders include influenza A or B, parainfluenza, respiratory syncytial virus, and rhinovirus. The incidence of bronchitis is higher in smokers, older adults, young children, and in the winter months. The cough initially starts as dry and nonproductive and after a few days usually becomes productive.
Pneumonia an inflammatory reaction usually caused by an acute bacterial, viral, or fungal infection. It may be preceded by an upper respiratory tract infection, ear infection, or eye infection. Individuals who have had surgery, smoke, drink alcohol, are immune suppressed, and have chronic respiratory or other debilitating illnesses pose a greater risk of developing pneumonia. Crackles that do not clear with coughing can be heard.
Asthma is an obstructive disease of the lungs characterized by airway inflammation and hyperreactivity. Asthma can be triggered by extrinsic factors such as mold, pollen, dust animal dander or by intrinsic factors such as stress, fatigue or exercise. Along with a cough, patients usually present with shortness of breath, wheezing, and chest tightness.
Chronic Obstructive Pulmonary Disease (COPD) is a progressive and irreversible syndrome characterized by diminished inspiratory and expiratory capacity of the lungs. It includes emphysema and chronic bronchitis. COPD is often associated with smoking. A chronic cough is associated with COPD along with a barrel chest, distant breath sounds, and tachypnea. An increase in sputum can indicate an exacerbation of COPD.
Additional Causes- There are numerous other causes of coughing including smoking, allergies, GORD, foreign body, croup, side effects of medications, inhalation injury, cancer, tuberculosis, cystic fibrosis and lung disease.
Chronic cough
Causes of persistent or relapsing cough
- asthmatics (young children may present with cough without wheezing)
- heavy smokers (beware cancer)
- small children with catarrh
- whooping cough / modified pertussis
- Mycoplasma pneumoniae (3 month cough) Rx erythromycin/clarithromycin or doxycycline 2w
- tuberculosis
- Post viral infection the cough may last for some weeks
Bronchiectasis
Chronic airways disease with bronchial dilatation, mucociliary impairement and recurrent bacterial infections.
http://hacking-medschool.com/bronchiectasis-children
Recurrent RTIs
Investigating recurrent RTIs in Primary Care BMJ 2009
Acute SOB
http://www.youtube.com/watch?v=hGBV3V3MZag
- Causes of breathlessness
- Respiratory – OAD, infection, effusion, pneumothorax, PE, restrictive airways disease, Ca
- Cardiac – CHF, arrythmia, CHD
- Anaemia
- CRF – acidosis / Kussmauls
- Hyperthyroidosm
- Hyperventilation/Panic attack
Pneumonia
Infection within the alveoli.
May affect the alveoli within one or more lobes (lobar pneumonia) or in a more patchy distribution (bronchopneumonia)
Patient presents with fever, malaise, myalgia, rigors, cough, pleuritic pain +/- purulent (yellow green) sputum +/- haemoptysis.
http://hacking-medschool.com/pneumonia-emergencies
CRB-65 score for CAP |
|
|---|---|
| Confusion | MSS<8 (new) |
| Urea | >7 (if available) |
| Resp Rate | >30 |
| BP | SBP < 90 or DBP <60 mm Hg |
| Age | >65 yrs |
| 1 point for eachmax score 4 for CRB65 and 5 for CURB65 | |
| Score 0-1 | Low risk – may be suitable for home treatment |
| Score 2 | Intermediate risk – probably needs referral needed |
| Score 3-4 | High risk – urgent referral to hospital |
| CRB is risk of death / need for admission score.Other features suggesting need for admission irrespective of score -comorbidityhypoxia satts <92% PaO2 < 8KPabilateral or multilobar involvement | |
CAP
http://hacking-medschool.com/cap-emergencies
http://hacking-medschool.com/cap
http://www.cks.nhs.uk/chest_infections_adult#-294272
Inpatient Management CAP – Tayside
- CAP Organisms
- Strep pneumoniae
- Haemophilus influenzae
- Moraxellia catarrhalis
- Atypicals
- Influenza A
- Unidentified
- Atypical pneumonias
- Legionella
- Chlamydia pneumoniae
- Chlamydia psittaci
- Mycoplasma
- Coxiella burnetti (q fever)
Treatment
Home Rx: Amoxicillin 1g tds or doxycycline 200mg Day 1 then 100mg od for total 7 days.
If referring urgently – amoxicillin 1g oral or benzylpenicillin 1.2g IV before transfer (IV chloramphenicol 1 g if allergy).
severe or non-responding – add clarythromycinn…… edit this
HAP
Pneumocystis pneumonia
Influenza (respiratory)
250textbooks/influenza-vaccine
Flu vaccination (respiratory)
250textbooks/influenza-vaccination
Antivirals for influenza |
|
|---|---|
| Tamiflu / Oseltamivir Relenza / Zanamivirneuraminidase inhibitors inhibit the replication of influenza A and B.They should be started within 48 hours of symptoms and continued 5 daysAmantadine has been available since the 1970s, but is effective only against influenza A | |
| Use | Non-vaccinated high risk individuals presenting within 48 hrs of onset of flu-like symptoms |
| At Risk |
|
| Adult dose | Oseltamivir (tamiflu) 75 mg 1 capsule bd |
| Pregnancy | Inhaled Relenza 2 blisters (10mg) bd (1xOP)If contraindicated or systemic Rx needed then use oseltamivir.Discuss risk/benefit in all cases. |
| Breastfeeding | Oseltamivir 75mg bd 5d(unless on Relenza for other reasons) |
| Children >1 |
|
| Children <1 | Oseltamivir liquid 15mg/1ml
|
| This was during Tamiflu shortage – particularly Tamiflu liquid and generic Osteltamvir was recommended instead for under 1s (unlicensed)– up to date??Prescriptions should be endorsed SLS | |
| Tamiflu Oral Suspension is 12 mg/ml |
| Oseltamivir Oral Solution is 15 mg/ml |
Pandemic flu
Severe acute respiratory syndrome SARS (respiratory)
http://hacking-medschool.com/sars
Tuberculosis TB
Due to droplet transmission of Mycobacterium tuberculosis from person with active pulmonary TB.
Primary TB
Post primary TB
Diagnosis
Tuberculin test (Mantoux and Heaf)
BCG vaccination
North West Medicines Information Centre Nice Bites Jul 11 Tuberculosis
Tuberculosis in the UK—time to regain control BMJ Jul 2011
Stopping routine vaccination for tuberculosis in schools BMJ 2005
Routine BCG vaccination of schoolchildren against tuberculosis stopped in 2005.
BCG vaccination will now be offered to infants in communities with an average incidence of tuberculosis of at least 40 per 100000 and to unvaccinated families from countries of similar incidence. Most people born in the UK now will not receive BCG. As most will not be exposed to mycobacteria, tuberculin testing will become more efficient in detecting infection.
NICE CG33 Clinical diagnosis and management of TB and measures for its prevention and control
Consolidation
Localised area of pneumonia (??) due to infection, infarction, malignancy.
Shows on X-ray as homogenous opacity with ill defined margins.
- Clinically
- Reduced chest movement on affected side
- No shift of trachea or apex beat.
- Increased vocal fremitus.
- Reduced percussion note
- Bronchial breathing
- Fine or coarse crepitations
- Increased vocal resonance
- Whispering pectoriloquy.
Lobar collapse
- Decreased movement and flattening of chest wall on side of collapse
- Trachea shift (upper lobe collapse) and apex shifted (lower lobe collapse) towards side of collapse
- Decreased PN
- Reduced breath sounds +/- bronchial breathing and creps if assosciated consolidation
- CXR shows homogenouus dense opacity. Lateral view may help locaise affected lobes.
Causes
- Obstruction of major bronchus by Ca, FB, lymph nodes or pus
- Lung compression by pleural effusion or pneumothorax.
Pleural effusion
| Pleural Effusion | ||
|---|---|---|
| Transudate | protein < 30g/lLDH < 200 iu/l |
|
| Exudate | protein > 30g/lLDH >200 iu/l |
|
Clinically
Decreased chest movements on side of effusion
Trachea and apex not shofted unless effusion is massive
Vocal fremitus reduced or absent
Absent or reduced BS
Absent Vocal Resonance
Bronchial breathing over upper level of effusion
Pneumothorax |
|
|---|---|
| Spontaneous | tall thin young men |
| Secondary | COPD, asthma, lung tumour or abcess |
| Traumatic | rib fracures, stab wound |
| Iatrogenic | central lines, transbronchial biopsy |
| Tension | insert canula immediately into 2nd intercostal space in MCL |
| Clinically | Sudden onset SOB and pleuritic chest pain in young thin individual.
|
Atelectasis
Fibrosing alveolitis
Idiopathic diffuse interstitial fibrosis characterized by dyspnoea, dry cough, clubbing, fine velcro crepitations in lower lungs.
Idiopathic Pulmonary Fibrosis PUK
Fibrosing Alveolitis Pulmonary fibrosis British Lung Foundation
Extrinsic allergic alveolitis
Inflammation of the alveoli and small airways (pneumonitis) due to a type III (delayed) hypersensitivity reaction to inhaled organic antigens – bird proteins, fungi and protozoa. The antigen must be small enough to be depositied in the distal lung. It becomes bound to circulating IgG forming immune complexes which then cause mast cell degranulation and inflammatory cell infiltration. Symptoms develop 4-12 hours after exposure.
Symptoms may also be subacute / insidious due to ongoing exposure, or chronic due to fibrosis.
Bird fanciers lung
Farmers lung
Humidifier fever
Maltworkers Lung
The alveolar and small airway inflammation impairs gas transfer and causes breathlessness and cough. Spirometry shows a restrictive pattern (reduction in lung volumes)
Extrinsic Allergic Alveolitis PUK
Extrinsic Allergic Alveolitis British Lung Foundation
Farmers Health Rural Health West
Pulmonary eosinophilia
Pulmonary eosinophilia umm.edu
Pulmonary eosinophilia medscape
Pulmonary eosinophilia Respiratory Reviews.com
Sarcoidosis
Chronic multisystem disorder characterised by development of non-caseating (cf TB) granulomas (small foci of chronic inflammation) particularly in the lungs skin and eyes.
May be asymptomatic or may present with respiratory symptoms, erythema nodosum, joint or opthalmic symptoms, hypercalcaemia.
- Staging of pulmonary sarcoidosis
- Stage 1 – bilateral hilar lymphadenopathywithout parenchymal disease
- Stage 2 – BHL with non-fibrotic parenchymal disease
- Stage 3 – Non -fibrotic parenchymal disease alone ( hilar glands have shrunk)
- Stage 4- fibrosis and distortion of lung
Other granulomatous disorders include TB Crohns aspergillosis and autoimmune disorders.
| Aspergillosis Aspergillus fumigates | |
|---|---|
| Aspergiloma | Growth of Aspergillus colony in existing lung cavity |
| ABPA | Allergic bronchopulmonary aspergillosisResistant asthma due to secondary immune reactions to Aspergillus colonisation of lungs |
| Invasive aspergillosis | severe disseminated/destructive infection in immunocompromised – AIDS steroids neutropaenia |
Drugs causing lung damage
Drugs causing lung damage Medscape
Immunological lung disease
slideshare.net immune mediated lung diseases
Occupational lung disease
Pneumoconiosis
Asbestos related disease
Pleural plaques
Asbestosis
Lung Cancer
Mesthelioma
Lung cancer
Lung Cancer Types
Non Small Cell
Respond poorly to chemo Rx – localised peripheral lesions may be cured by surgery.
Squamous Cell 35-45%
Adenocarcinoma 15%
Large cell carcinoma 10%
Carcinoid 1%
Bronchoalveolar cell carcinoma
Small cell (20%)
endocrine (APUD) derived fast growing highly malignant metastasises early
Lung cancer staging
Lung Cancer Treatment
NICE CG24 Lung cancer Feb 2005 QRG
Therapeutic advances in non-small cell lung cancer Thorax Nov 2011


